-
Ventilators
Magnamed Fleximag Max Ventilator
Original price was: ₹1,600,000.00.₹1,450,000.00Current price is: ₹1,450,000.00. -
Ventilators
Magnamed Oxymag Ventilator
Original price was: ₹1,050,000.00.₹850,000.00Current price is: ₹850,000.00. -
Ventilators
Philips Trilogy Evo (OBM) Ventilator
Original price was: ₹760,000.00.₹680,000.00Current price is: ₹680,000.00. -
Ventilators
Resmed Astral 100 Ventilator
Original price was: ₹403,000.00.₹345,000.00Current price is: ₹345,000.00. -
Ventilators
Resmed Astral 150 Ventilator
Original price was: ₹652,000.00.₹455,000.00Current price is: ₹455,000.00. -
Ventilators
Resmed Stellar 100 Non Invasive Ventilator
Original price was: ₹215,000.00.₹193,500.00Current price is: ₹193,500.00. -
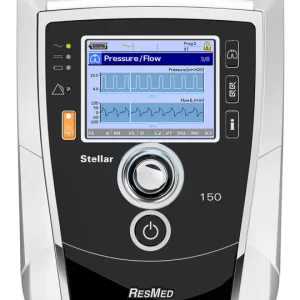
Uncategorized
Resmed Stellar 150 Non Invasive Ventilator
Original price was: ₹350,000.00.₹224,000.00Current price is: ₹224,000.00.
A medical ventilator is a machine that helps your lungs work. It can be a lifesaving machine if you have a condition that makes it hard for you to breathe properly or when you can’t breathe on your own at all.
A ventilator helps to push air in and out of your lungs so your body can get the oxygen it needs. You may wear a fitted mask to help get oxygen from the ventilator into your lungs. Or, if your condition is more serious, a breathing tube may be inserted down your throat to supply your lungs with oxygen.
Ventilators are most often used in hospital settings. A doctor or a respiratory therapist will control how much oxygen is pushed into your lungs by the ventilator.
Other names that a ventilator is known by include:
- Respirator
- breathing machine
- mechanical ventilation
Not being able to breathe properly on your own is known as respiratory failure and is a life-threatening emergency.
If your brain, heart, liver, kidneys, and other organs don’t get enough oxygen, they won’t be able to function as they should. A ventilator can help you get the oxygen you need for your organs to function.
Health conditions
Many types of health conditions can cause you to have difficulty breathing, such as:
- acute respiratory distress syndrome (ARDS)
- chronic obstructive pulmonary disease (COPD)
- asthma
- brain injury
- cardiac arrest
- pneumonia
- collapsed lung
- stroke
- coma or loss of consciousness
- drug overdose
- hypercapnic respiratory failure
- lung infection
- myasthenia gravis
- sepsis, an infection in your blood
- upper spinal cord injuries
- premature lung development (in babies)
- Guillain-Barré syndrome
- amyotrophic lateral sclerosis (ALS), commonly known as Lou Gehrig’s disease.
You may be put on a mechanical ventilator, also known as a breathing machine, if a condition makes it very difficult for you to breathe or get enough oxygen into your blood. This condition is called respiratory failure.
There are several ways a person can receive ventilator support. These include:
face mask ventilators
mechanical ventilators
manual resuscitator bags
tracheostomy ventilators
Face mask ventilators are noninvasive, while mechanical and tracheostomy ventilators are invasive and work via tubes that a doctor inserts through a hole in the neck that leads to the trachea, or windpipe. Healthcare professionals term this intubation.
For some, a face mask ventilator may be sufficient to stabilize their condition. People who physically struggle to breathe independently may require mechanical ventilation.
Below, we look at each type of ventilator and how they work.
Face mask ventilator
A face mask ventilator is a noninvasive method of supporting a person’s breathing and oxygen levels. To use one, a person wears a mask that fits over the nose and mouth while air blows into their airways and lungs.
People with COVID-19 may use a face mask ventilator if they are having difficulty breathing or do not have sufficient oxygen levels.
Continuous positive airway pressure (CPAP) and bi-level positive airway pressure (BiPAP) devices also operate via a face mask.
People often use these for chronic conditions, such as chronic obstructive pulmonary disease, but some doctors may also useTrusted Source them for people with COVID-19.
In addition to supporting oxygen levels, PAP therapy can also aid in expelling carbon dioxide levels. Whether a doctor decides to use CPAP or BiPAP will depend on a person’s underlying condition.
Mechanical ventilator
Mechanical ventilators are machines that take over the breathing process entirely. Doctors use these when a person cannot breathe on their own.
Mechanical ventilators work via a tube in a person’s throat, pumping air into the lungs and transporting carbon dioxide away.
A ventilator unit regulates the pressure, humidity, volume, and temperature of the air, depending on the controls that a doctor or respiratory therapist places. This allows healthcare professionals to control a person’s breathing and oxygen levels.
People with COVID-19 may need a mechanical ventilator if they are critically ill.
Manual resuscitator bags
Manual resuscitator bags are pieces of equipment that allow people to control the airflow of their ventilator with their hands. These devices consist of an empty bag, or “bladder,” that a person squeezes to pump air into the lungs.
A person can attach one of these devices to a face mask ventilator, or, if they are intubated, a doctor can attach one to the tube in their throat.
This can be useful as a temporary solution if a person on a mechanical ventilator needs to stop using it. For example, if there is a power outage, a person can use a manual resuscitator bag while waiting for the power to come back on.
Tracheostomy ventilator
People who have undergone a tracheostomy will require a ventilator.
A tracheostomy is a procedure where a doctor creates an opening in the windpipe and inserts a tube, which allows air to flow in and out. This enables a person to breathe without using their nose or mouth.
People who have undergone tracheostomies can also receive ventilator support through this opening. Instead of inserting a ventilator through the mouth, doctors insert it directly into the windpipe.
People may require tracheostomies if they need mechanical ventilation for an extended period of time and need more time for rehabilitation.
Others may require tracheostomies long term if they have conditions such as chronic lung disease or a neuromuscular disorder that weakens the breathing muscles. Some individuals can manage their own tracheostomy at home.
Ventilator types are broken up into two categories: noninvasive ventilators and invasive ventilators.
Noninvasive ventilators provide breathing support through an external interface, such as a mask or nasal prongs. These are positive airway pressure ventilators that use positive pressure to force gas or air into a patient’s lungs. Breathing can be triggered by either the patient or the machine. There are six types of positive pressure ventilators.
Volume-cycled ventilators—deliver a preset volume of gas/air or a “tidal” volume and allow passive exhalation. This is ideal for patients with acute respiratory distress syndrome or bronchospasm.
Pressure-cycled ventilators—deliver gases at a preset pressure and allow passive exhalation. They decrease the risk of lung damage from high inspiratory pressures. A disadvantage is that the tidal volume delivered can vary with changes in lung resistance and compliance if the patient has poor lung compliance and increased airway resistance. It is often used in short-term therapy.
Flow-cycled ventilators—deliver oxygenation until a preset flow rate is achieved during inhalation.
Time-cycled ventilators—deliver oxygenation over a preset time period. These are not used as frequently as the volume-cycled and pressure-cycled ventilators.
Continuous positive airway pressure ventilators—increase the work of breathing by forcing the user to exhale against resistance. Because this ventilator provides a continuous flow of air at the same level of pressure during inhalation and exhalation to keep the airway open, it is ideal for treating obstructive sleep apnea. This type of ventilator is not considered a true ventilator because it doesn’t assist with breathing.
Bi-level positive airway pressure ventilators—deliver air at two pressures for inhalation and for exhalation. They help treat neuromuscular disease with a spontaneous timed mode or backup rate that initiates breathing, particularly at night.
Invasive ventilators deliver air through an endotracheal tube inserted into the patient’s nose or mouth, or through a tracheostomy, a surgical incision in the neck to access the trachea. Air is delivered on a timed cycle through the tube and ensures that the patient takes a minimum number of breaths per minute. These ventilators can be adjusted to respond to the patient’s own efforts to breathe or to override these efforts.
Top 5 Ventilator With Price In India
- Drager Savina Ventilator
- Nidek Oxymag Ventilator
- Resmed Astral 150 ventilator
- Philips Trilogy EVO ventilator
- Nidek Fleximag + Ventilator
Ventilator Price in India
- Drager Savina Ventilator ₹ 120,0,000
- Nidek Oxymag Ventilator – ₹ 650,000
- Resmed Astral 150 ventilator – ₹ 550,000
- Philips Trilogy EVO ventilator- ₹ 650000
- Nidek Fleximag + Ventilator – ₹ 12,00,000
Buy ventilators at the lowest price from MG Medicare. We provide 100% genuine ventilators with original accessories . .MG Medicare is the best online and offline medical equipment supplier in India. It offers the lowest ventilator prices for hospitals, clinics, nursing homes, and patients. It provides the best quality and support with an award-winning customer care team. With us, you will find the best ventilators in India. For offline stores, you can visit your nearby stores in New Delhi and Lucknow. Call us 9310629328 for the best price and products or mail at [email protected]